This guide is intended to be a brief overview of common issues and questions that have come up during the attestation process. If you have further questions regarding your specific situation, please reach out to our customer service department to schedule an individual training session. This guide also includes training videos to help guide you through this process.
Minimum required to avoid 2019 penalty
- Complete all ACI Base Score Measures OR
- Complete 1 Quality Measure OR
- Complete 1 Practice Improvement Activity
Choosing your Attestation Time Period
- Minimum of 90 days
- Allowed to choose different reporting periods for ACI – Quality – IA
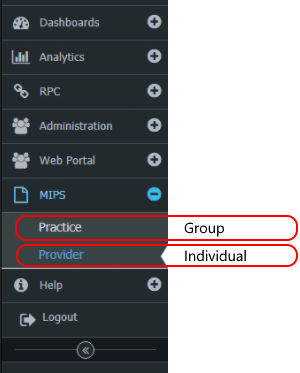
Group vs. Individual Reporting
- Whatever you choose it needs to be the same for ACI – Quality – IA
- Group reporting is based on the Tax Identification Number (TIN)
- Group reporting can be helpful if you have a mixture of MD’s and OD’s
Selecting Improvement Activities
- For practices with under 15 providers, you need to select at least 2 medium weighted measures or 1 high weighted measure
- For practices with 15 or more providers, you need to select at least 4 medium weighted measures, 2 high weighted measures, or 2 medium and 1 high
- Make sure you read the measures completely and have proper documentation to prove compliance if audited.
- Read the AAO Improvement Activities Guide for guidance on selecting measures that fit your practice
Security Risk Assesment
- Review and update existing security risk assessment prior to attestation
- If you have never completed an SRA before or need to complete a new one, download the tool here
Attesting with IRIS vs. QPP Portal
- IRIS deadline for submission is January 31st – QPP deadline for submission is March 31st
- If you report through IRIS, you can also report through the QPP portal later if needed
Tips when attesting with IRIS
- Enter the CHPL ID of 027712 when prompted
- Review all questions carefully, especially the question related to practices under 15 providers
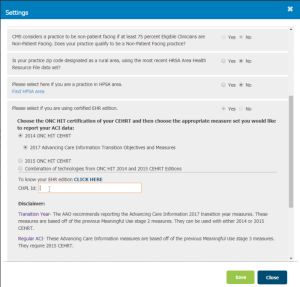
- Select 2014 ONC HIT CEHRT – 2017 Advancing Care Information Transition Objective and Measures
- When asked if you write less than 100 E-Rx, only select yes if you plan on taking the exemption
- When asked if you write less than 100 referrals, only select yes if you plan on taking the exemption
NOTE: Taking an exemption excludes you from using that measure for the performance score
- Make sure you enter your information under the correct area depending on how you plan to report
Tips when attesting on the QPP Portal
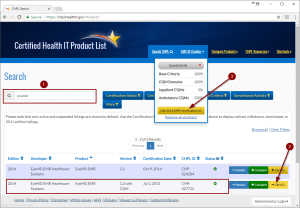
- Select the proper Certification ID from the Certified Health IT Product List
- Search for your EHR by name
- Click the +Cert ID button to add it to the CMS ID Creator
Repeat steps 1 and 2 for any additional EHR products that you use
- Click the Get EHR Certification ID button then click Download PDF
Watch the latest MIPS webinars!
- Click here to watch the CMS MIPS Attestation Training
- Click here to watch the EyeMD EMR MIPS Attestation Training

 EyeMD EMR Named 2024 Best In KLAS: Ambulatory **Ophthalmology** EMR
EyeMD EMR Named 2024 Best In KLAS: Ambulatory **Ophthalmology** EMR